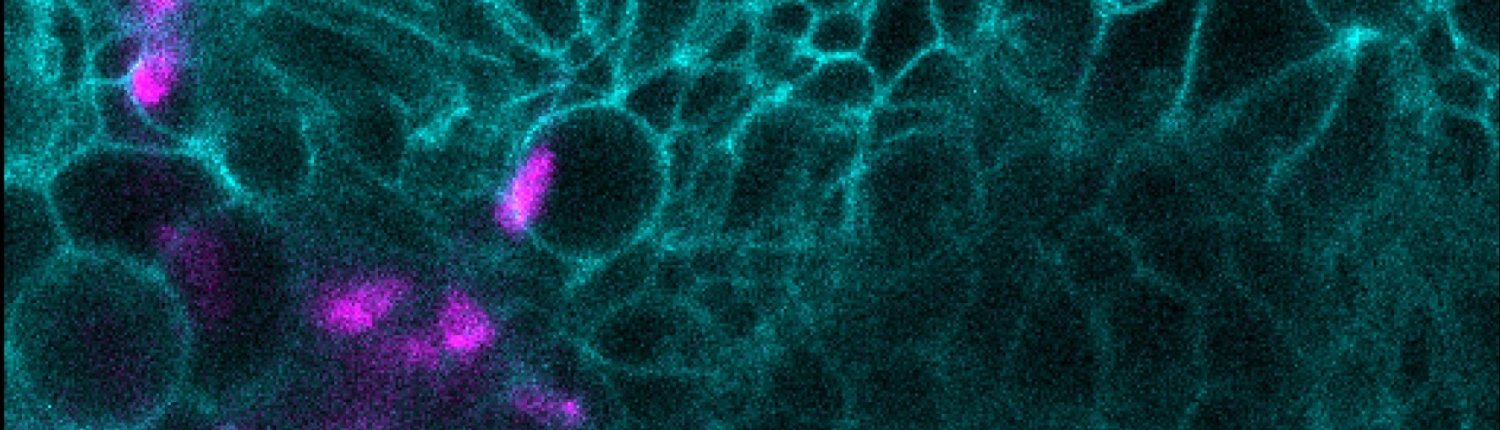
Immune cells serve critical roles in maintaining organisms in a healthy state, interacting with both interlopers and internal targets. They eliminate infections by bacteria, viruses and parasites. Recent studies have shown that they also regulate processes of development, repair and regeneration, altering stem cell behavior and modulating metabolism. These functions depend on immune cells entering tissues, some during development to become tissue resident macrophages, such as microglia, and some in the adult in response to infection or damage, such as monocytes and neutrophils. Despite its importance, this is an extremely underexplored area.
We identify the cellular components and processes that regulate tissue invasion as a first step towards modulating this capacity. We particularly relish identifying unknown cellular pathways. Tuning infiltration up or down in a localized fashion could potentially decrease autoimmunity, improve immuno-oncological approaches to eliminate tumors, and increase regeneration and repair of damaged tissues.
We also explore our pathways’ broader physiological relevance, including a new regulator of mitochondrial function, and other macrophage-tissue interactions.
We ask:
1) In what ways does the tissue itself control infiltration?
2) What programs are required inside infiltrating cells for tissue invasion?
3) Do our pathways control other aspects of immune and neural function?
Approach:
We use a combination of diverse techniques (in vivo imaging, genetics including CRISPR/Cas9 modification, cell biology, mass spectrometry, metabolomics, next generation sequencing, biophysics and modeling) to identify the mechanisms that underlie tissue invasion. We utilize Drosophila macrophages in the embryo as a model system to discover novel pathways, and extend our findings through collaborations to vertebrate models, including mouse, zebrafish, organoids and human cells.